How does educator-supported referral work?
The PSW Referral Form should be completed by the educator after a discussion with the resident doctor in postgraduate training about the reason(s) for the referral to PSWS and the support being requested. The form should not be submitted unless both the doctor and educator agree about the referral. A copy of the form will be sent to both the referrer and resident doctor in training after it has been reviewed by the PSW team.
This approach provides an opportunity for the educator and resident to explore together any issues, and enables space for support to be offered at local level first. This then provides a good foundation from which the resident can be supported to access PSWS support.
Who should be the educator supporting the referral?
Often the resident will feel comfortable sharing the issues impacting their training with their Educational Supervisor. However, for many different reasons there may be another educator who is better placed to provide the support. This may be the Clinical supervisor, College Tutor, Training Programme Director, Head of School or Director of Medical Education.
What is of paramount importance is that the resident feels comfortable sharing with the educator and receiving that local support. In the rare circumstance that a particular resident does not feel able to share at local level, they can approach PSWS for a confidential conversation with the TPD or Associate Dean for PSWS.
What happens following a referral?
Please see Trainee FAQs.
How do I recognise when a resident doctor is struggling?
Signs that a doctor is struggling are varied. These may be: issues relating to their clinical performance; behavioural concerns; sickness; life events; work-place environmental problems; or poor engagement.
Being specific about the impact on the doctor’s work performance is important. Examples:
Work based – Absence from duty, persistent lateness, poor time-management, backlog of work, failure to learn and change.
Clinical performance markers – Over or under-investigating, poor decision-making, poor record-keeping, complaints, failure to follow guidelines, missed diagnosis.
Psychological/Personality – Irritability, unpredictability, forgetfulness, highly self-critical, perfectionism, arrogance, lack of insight, denial, risk-taking, impulsive.
Social – Isolation, withdrawal, poor personal interactions.
Cognitive – Memory problems, poor problem-solving, poor reasoning, poor decision-making, poor concentration, lack of attention, learning problems.
Language/Cultural – Poor verbal fluency, poor understanding.
This information has been adapted from the report, Practitioner Performance Advice (formerly the National Clinical Assessment Service, NCAS) meeting on Doctors in Difficulty: Firth-Cozens, 2004.
Elizabeth Paice (2006) identified Seven ‘Early Warning Signs’:
The ‘Disappearing Act’ – not answering bleeps; disappearing between clinic and ward; lateness; frequent sick leave.
Low work rate – slowness in doing procedures, clerking patients, dictating letters, making decisions; arriving early, leaving late and still not achieving a reasonable workload.
‘Ward Rage’ – bursts of temper; shouting matches; real or imagined slights.
Rigidity – poor tolerance of ambiguity; inability to compromise; difficulty prioritising; inappropriate „whistle blowing‟.
‘Bypass Syndrome’ – junior colleagues or nurses find ways to avoid seeking the doctor’s opinion or help.
Career problems – difficulty with exams; uncertainty about career choice; disillusionment with medicine.
Insight failure – rejection of constructive criticism; defensiveness; counterchallenge.
When would a resident doctor requiring additional support benefit from a referral to the PSWS?
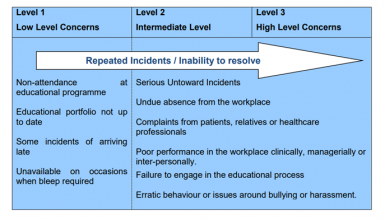
Broadly, there are three escalation levels for concerns, and who needs to know depends on the level of concern. Prior to referral to PSWS, it is expected that there has been confidential discussion with appropriate colleagues within the Trust or Specialty School, with consequent additional support offered to the trainee. Documentation of concerns, actions and related correspondence is imperative, as is openness and transparency in discussions with the resident.
Level 1 Low Level Concerns – Educational Supervisor
Level 2 Intermediate Level Concerns – also needs support network in Trust or Specialty (e.g. Director of Medical Education, College Tutor, Training Programme Director or Head of School)
Level 3 High Level Concerns – also needs PSW referral
Any trainee where there are serious and/or repeated performance problems (health, conduct or capability) must be referred to PSWS.
When should a referral to Occupational Health be made?
The Occupational Health service in each Trust can advise on the impact of both work on health, and of health on work. It is important to take advice when a resident doctor’s health is considered to have the potential to negatively impact patient safety. Advice should also be sought in order to help decide on the appropriateness, and manner, of a return to work, after sickness absence. If it is considered that a resident doctor’s health may be an issue for their work, it is best to seek advice early.